DISCUSSIONS ON FECAL TRANSPLANT
Before my retirement from the clinical practice of Gastroenterology, a female patient (who was a relative of a Bell Labs research scientist) had recurrent C. Difficile Colitis and was transferred to my service from a nursing home. She has been on oral antibiotics for a chronic urinary tract infection.
The possibility of treating her with fecal transplant (FT) was raised during treatment discussions. The research scientist, the relative of the patient, with his exquisite mind has raised many probing and relevant questions about a fecal transplant. I was not able to answer them, and I still do not know the answers to his questions. I would like to share his questions and some of my thoughts with my readers, with the hope that some experts on the subject will answer them. The questions were as follows:
1. Why do you call it transplant, isn’t transplant an utmost sterile surgical procedure that is done after extensive compatibility studies, tissue and blood typing? You are not transplanting stools. You are simply transferring very unsterile stools which contain many live and dead bacteria, fungus, viruses and toxic excreta. Wouldn’t it better to call it stool transfer, instead of saying stool transplant?
2. Since no stool compatibility studies are done, wouldn’t it be better to obtain fresh stools from healthy and close relatives? This stool would have a better chance to be compatible with the patient. Shouldn’t this be a required standard for so called stool transplant?
3. You are not trying to transplant stool; you are trying to transplant beneficial microbiomes in the stool. The word “stool or fecal” should be eliminated from the procedure, and it should be called microbiome transfer or transplant.
4. Since C. Difficile Colitis occurs after treating an infection with oral antibiotics, why are you giving stronger antibiotics to kill C. Diff infection? Wouldn’t that also kill more beneficial bacteria and cause more or recurrent C. Diff infections?
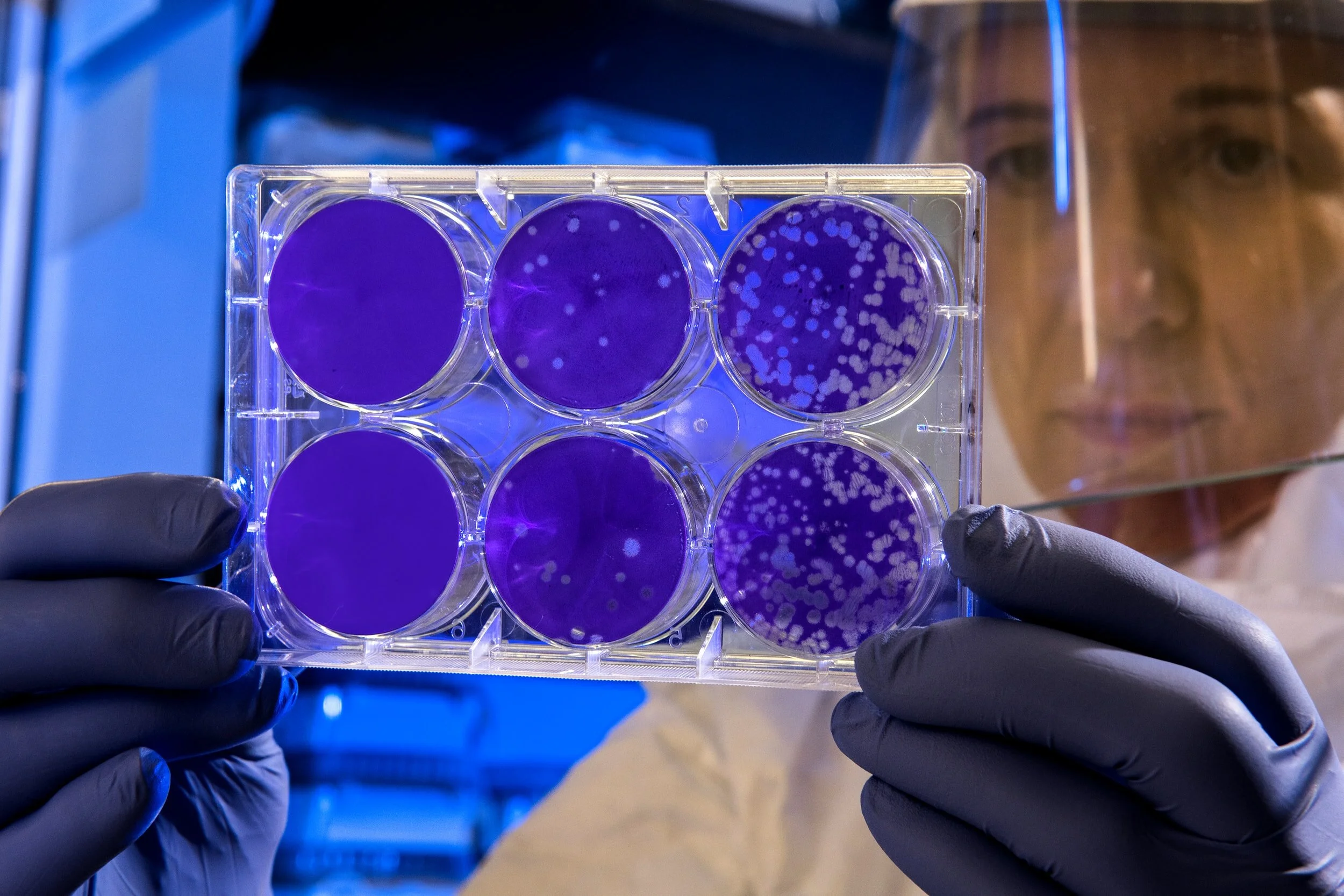
5. Are beneficial bacteria populations the same in every person? Could they be identified, isolated and cultured in the laboratory and given to the patient instead of transferring the whole stool? Shouldn’t this be the norm?
For Further Reading: ”Development of Human Derived Intestinal Microbiota for Prevention of Recurrent C. difficile Infection” on VUMedi by M. Woodworth, MD